
October 2022
So It Appears I Finally Have A Plan…
Houston, it appears I finally have a plan. Sort of.
This week I met with the generous vascular surgeon Kurtis Kim, (thanks to a grant from a grateful patient of his) and a bariatric surgeon from UCHealth, Dr. Akshay Chauhan. Between them (and more than a decade of plodding around on the ground doing research and interviewing dozens of docs,) I seem to have been catapulted into a world which matches (or tries its best to match) symptoms, testing, medical imaging and surgical plans.
There is still some flux on the question of which vascular compressions I “have” and “don’t have.” Colin and I recently posited that perhaps, like Schrodinger’s cat, I exist in two universes, one in which I have no compressions and one in which I have …all of them? Perhaps I fluctuate between these universes.
Well, anyway, let’s review the cast:
Compressions:
NCS – Renal Nutcracker Syndrome, compression of the renal vein between the abdominal aorta and SMA (auperior mesenteric artery)
MTS – May-Thurner, compression of the left common Iliac vein
MALS – Median Arcuate Ligament Syndrome, compression by the median arcuate ligament on the celiac artery (neurogenic and vascular types available)
Eagle Syndrome – Elongation of the styloid process, mine is the jugular variant, causing compression of the internal jugular vein.
Vena Cava – Compression of the vena cava
Supporting cast:
EDS – Ehlers-Danlos Syndrome, a genetic condition of the collagen, affecting connective tissue. I have the hypermobile type.
POTS – Postural Orthostatic Tachycardia Syndrome – characterized by fatigue, lightheadedness, low blood pressure and tachycardia on standing.
Nephroptosis – In which your kidneys drop when you’re standing.
MCAS – Mast cell activation Syndrome
Dr. Scholbach, who I saw in Germany, believes I have all the above compressions except MTS. Dr. Garland thinks I have only SMAS. Dr. Kim, (who is perhaps on his way to becoming the American Dr. Scholbach, but the vascular surgeon version, as opposed to the pediatrician who kind of fell into this world out of frustration for lack of care) doesn’t really think vena compression is a thing, and nephroptosis is over-diagnosed. However, he does believe I have NCS, MTS and possibly MALS.
In the past ten years I’ve had about a dozen opinions, all in between. I had CT scans, MRIs, several ultrasounds, an Intravascular Ultrasound… I was even a patient model at a vascular conference. 100% disagreement on all fronts. The doc who took me under his wing at the vascular conference suggested maybe I have Lyme disease. (Which now seems true, but beside this point.)
Dr. Chauhan, who I saw yesterday, looked at my most recent CT scan and had a couple observations. First, “Oh, that’s definitely MALS, look at that, it’s so obvious, there’s this huge glob of tissue sitting right there on the artery; that’s not normal!” Pointing to a fluffy white blob of which looks like all the other fluffy white blobs on the screen to me. No surprise, no one else except Scholbach has suspected this.
Second, (and this is where I think I might give myself a tiny little victory lap,) he compared my duodenum from a CT in 2017 to last weeks. “Look at this, it’s much more normal now – did you gain weight?” Yes, yes I did. My duodenum, which in 2017 took up a huuuuge portion of my upper right quadrant, (probably because it was pinched off further downstream at the SMA,) now appears about the size of one of my hands. Normal! It seems I may have successfully regained the fat pad which supports the SMA angle, which can pinch the duodenum when it’s too tight. Now, perhaps, I may enjoy a less painful digestive process.
Arrow points to duodenum in 2017:
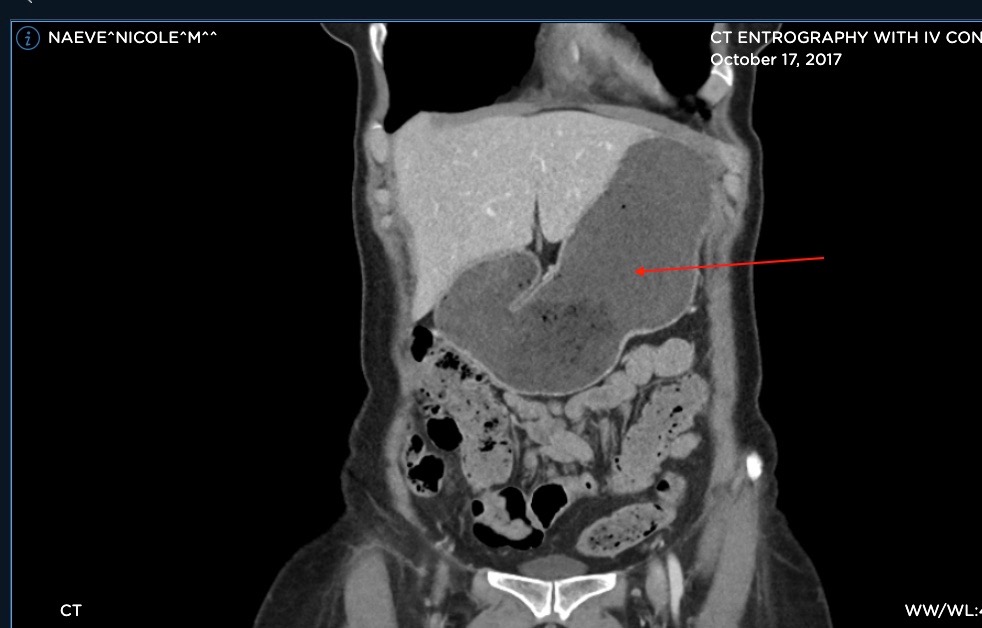
Below, arrow points to duodenum in 2022
Many SMAS patients, particularly young women, end up in pscyh hospitals because the medical establishment assumes they’re anorexic. They cannot distinguish because someone who refuses to eat from someone who is afraid to eat because it hurts. Others (perhaps luckier) get feeding tubes. In 1995 I got really sick in Bali and would double over after eating anything. There was a spot of intense pain, just to the right of my Xyphoid process, my friends and I named “Gerald.” I’m not sure why – perhaps at some point somebody suggested it might be Giardia. I chased an immunological source of my distress for decades – parasites, (protozoan, viral and bacterial,) autoimmune disease, liver flukes, hepatitis…all were turned over and examined. I sent poop off to several labs, had testing for autoimmune disease,
swallowed cameras, had dozens of tubes of blood looked at under microscopes. We found things, like Hashimotos and EDS, but never things which really helped.
I didn’t have anybody to tell me anything, so I drank lots of Spirutein and Ensure. If I needed energy to get through my massage workday I’d eat a something like a Snickers bar, verrry slowly, chewing like a hundred times. In the evenings, if I didn’t have rehearsal, I’d eat a regular sized meal and get myself immediately into a warm bath, which would somehow help me alleviate some of the pain on eating.
That helped me gain a little weight, and maintain at around 125lbs for several years. I gradually increased my capacity to eat, but progress wasn’t linear. I’ve had bouts of painful eating ever since. Meanwhile I’d be diagnosed with multiple autoimmune diseases, EDS, POTS, interstitial cystitis, etc.
For my most recent weight gain I credit quitting the theater, (or as it’s known in the business, I’m “resting!”) moving to a place where people enjoy a commuter lifestyle (anywhere you go in NY requires stairs, walking, then more stairs and walking; Colorado you exercise in the mountains when you choose) making eating and sleeping in a calm, relaxed environment and giving myself as much time to eat and sleep as I need a priority and lastly, menopause. Oh, sweet menopause, which also reduced my pelvic pain by about 80%.
Say what you will about the down sides of aging. I’ll take it. I now sit smack in the middle of “normal” weight for my age and height – 142lbs – and I have curves! Lucious and curvy curves I haven’t enjoyed since high school. I’ll never complain about a little pudge under the waist again. Eat that, vascular compressions!
So the next step is a diagnostic test for MALS, in which we block the nerve bundle which is the celiac plexus, and see if that reduces my symptoms. Assuming that’s positive, we move forward with a surgical plan to cut the median arcuate ligament to free the celiac artery and, while we’re at it, remove the gallbladder.
Oh, the gallbladder. I’ve been holding onto it for the past several years, knowing its ejection fraction is only 17% (anything under 35% is considered grounds for its permanent dismissal) but thinking perhaps it’s reacting to something up or downstream, so could fix itself some day. Well, I’ve been doing some research and it’s not looking good for the poor gallbladder. It seems that most people with MALS have the same “lazy” gallbladder issue I do, and it rarely, if ever, bounces back, even after fixing the MALS. Dr. Chuhan proposes to take it in the same surgery, along with the celiac plexus nerves which might remember it ever existed.
I’ve already got Eagle syndrome surgery on the books for January 18, 2023. (It was cancelled last January due to Covid, and that office books way ahead.) The plan? Fix a deviated septum, clear a chronic sinus infection, move along the entire right jugular and clear anything which might impede its flow, including adhesions, the styloid process, and maybe gremlins? Also – and this is kind if the biggie – check and see if that teeny hole behind my right nostril is leaking CSF fluid, and if it is, glue a patch on it.
Fixing that CSF leak is my biggest concern. It may currently be acting as a “release valve” for increased intracranial pressure due to compression at the renal vein. That kidney is under a ton of hydrodynamic pressure. So… Fixing that could increase headaches.
But it may not even be leaking. Or, if worse headaches do happen, it could be evidence in support of the NCS, and help get me past the “gatekeepers” for the surgeons for NCS.
I’ve had some trouble, there. My local Denver option is to move or remove the kidney, but I failed their testing. I’d actually prefer a surgical technique which might address both NCS and SMAS, anyway, which would be to place an external “stent” or “sheath” around the renal vein, protecting it and increasing the SMA angle into which it is pinched.
There are two surgeons in the US who do this. One’s gatekeeper told me he’s looked at my imaging and notes, and thinks I should pursue getting “all compressions addressed in one surgery.” Not possible in the US. I could go to Germany and spend 40K with Dr Sandmann, who is 80 years old and while really good at NCS surgery, maybe isn’t so good with MALS and average on MTS. Did I say this to the gatekeeper? Yes. Did I ask her to relay this to the doctor? Yes. Have I heard back? Of course not.
The other, in Dallas, won’t do telehealth with anyone out of state. I’m in talks with the hospital’s presidential office to try and make an exception. Or I may go to Dallas for a chat with him.
Alternately, there’s Dr. Nagarsheth in CT, who does open NCS surgery where he re-arranges vessels, and he can place a stent in the iliac vein in the same surgery.
So, THE PLAN, as it stands, is multiple surgeries/procedures, spaced out by 2-4 months:
1) Celiac plexus block
2) Eagle surgery, plus head stuff.
3) MALS surgery, plus gallbladder ousting (assuming the celiac plexus block is positive) 4) NCS and perhaps MTS.
5) Perhaps pin a kidney or two.
I reserve the right to change this plan, either because it’s logical or because I freak out at any point along the way. With multiple surgeries something is bound to go wrong along the way, so changes can, and probably will happen. I also haven’t made a final choice on surgeons for 3, 4 and 5. I’ll likely have to travel for at least two. Salt Lake, Dallas, Columbus and CT are all possible at this point.
About this kidney “pinning,” Dr. Kim believes nephroptosis is overdiagnosed, and nephropexy (where they pin your kidney, I think to a muscle in your back, to keep it from dropping) should only be considered if yours drops over 5cm when standing. My right kidney drops 5.1cm, according to
Scholbach, so that’ll be a low priority, but still a consideration. When it drops, it can yank on the renal vein, further compressing it.
Meanwhile, my PT has to fire me because I’m not “progressing.” Insurance is a strict overseer. This is a real bummer because my PT keeps me functional, and keeps pain levels under control. I notice a distinct pattern of pain levels dropping after treatment, then gradually ramping back up until I see her again the following week. For some of us, lack of back-sliding IS progress. It’s like she’s dumping out the garbage. At your house, see what happens if that truck doesn’t drive up and pick up the trash once a week. 🙂
We’re going to take a break and then perhaps can start again. Or maybe I can find another miracle PT like my last one, who was willing to take more risks with insurance. Meanwhile I’ll budget for more private-pay bodywork.
Currently Dr. Kim is trying to assemble a “dream team” of doctors to treat vascular compression patients. He wants to create a space for a group of specialists who can consult on a single patient with multiple compressions (as we often present) and make a comprehensive surgical and treatment plan for them. He wants a great surgeon for each of the compressions – MALS, NCS, Eagle, etc. – a POTS person, an EDS person, an MCAS person, etc. He’s hoping – but making no promises – to do this in the next year or two, maybe in Virginia or New York.
He needs funding and support. I SO wish him well. We’re not sure exactly what the long-term effects of not treating vascular compressions are, (doesn’t appear to have been studied) but Dr. Kim has said, “Imagine if the main highway through a major city was stopped, and everyone is using side roads. That’s a very inefficient system.” It makes common sense that leaving these things to fester creates stress on the heart, markedly increases general fatigue and, of course being in chronic pain is not good for the body. Many suffer from malnutrition, but I seem to be past that.
I’d be ever so grateful if I could even just get rid of the stabbing pain, like I’ve been buttoned front to back, just under and to the right of the xyphoid process/diaphragm, which has hurt (and made eating hurt) since 1995. And there are probably a dozen more unknown consequences to leaving these conditions unchecked. Do those consequences outweigh the risks of multiple surgeries? Good question.
Meanwhile, I’m beginning to weave myself a little cocoon. Preserving vegetables in the garden in the form of frozen single-serving soups to eat while recovering. Stocking up on anti-nausea meds and ginger tea. Making a list of what to pack for overnight hospital stays. Reigning in travel, social and musical plans.
Oh, musical plans – Ben and I are currently working on Single release #2, “Lalita” – dare I hope we could get a third in before that first surgery? Maybe something simple….
And I’m allowing the tight fist of my imagination to begin envisioning what it might be like to be on the other side of all this. When I emerge from the cocoon, will I have more colors? Less pain? Will I flex my wings? Will I fly or fall in the breeze? I will still have hEDS and probably autoimmune disease, though perhaps I can take some stress off all systems. I sit in hope.
Love to all! Niki
Below: My CT from Sept. ‘22
Right arrows – SMA squishing renal vein & duodenum Left arrow – MALS “situation”


a) Normal SMA angle
b) abnormal SMA angle








Leave a comment