The Body Beat
August 2023
Hello and happy summer, everybody!
I know no one will read this whole thing, and that’s very much all right. Yes, I write these things to have my wounds kissed, but just as much to organize and crystallize information in my own head.
The medical stuff makes more emotional sense when it’s named, organized and codified in some way, its bones outlined in black and white, so when something hurts I can point to it and say, “Oh yeah, that alarm going off is because of that foraminal stenosis at C5-6, I get it. I send you, spine, some much needed compassion and love.” Or when I’m tapped out and exhausted I can picture all the little hormones and neurons and mitochondria inside, running on teeny treadmills and speeding from synapse to synapse as fast as their little feet will carry them, working so hard for me, and I can try to not be the asshole boss, demanding they work harder than they possibly can, to please me and my fulfill my (sometimes less than worthy) goals. I can speak to them, saying, “thank you for doing your very best for me.” And then I can move on.
So thank you all, inside, outside and everywhere, for doing your best, for yourself, for me, for your family, your worthy goals and just for plain being there.
I’m aware some of my tribe are medically curious and want to dig a little further down than others. For everyone else, perhaps the first sentence of every paragraph is enough to outline the situation.
There’s been a fair amount of activity on the diagnostic front for the Niki body these past few months. I keep waiting to write an update until it’s all “more clear,” but reality intrudes and delays abound. It seems what used to take 1-3 phone calls to arrange now takes 5-10 phone calls, 3 emails and as many FAXes. THEN you start over again when no one on the other end responds, or they stop taking new patients, or whatever. Everything has to be followed up and pursued with vigor, which happens to be the thing I most lack.
Genetics
So, if you’re a blood relative of mine, this may be the part to pay attention to. This is one thing I especially wanted to further clarify before passing on, but now I think this may just be where we are in medical science today – our understanding is fuzzy and evolving.
At the moment, I’m hearing conflicting information about how significant the “likely pathogenic” gene anomalies are for a mere carrier. Two doctors tell me that I could be manifesting symptoms of the pathogenic things I’m a carrier for, even though I don’t “have” the disease associated with them. Meanwhile a third tells me this is impossible – if you’re merely a carrier, you cannot manifest any symptoms. A little reading tells me this is a current controversy in genetics today. I have an appointment with a geneticist coming up – maybe that will add some clarity, but most likely will throw more sticks on the fire and make more smoke.
It’s further been explained to me that there are three different ways a gene can be “misspelled;” they can be deleted, added or transposed to another gene. If deleted or added, it’s far more likely for the carrier to manifest symptoms associated with that gene, than if it was just moved someplace else.
Here’s a summary of my recent genetic testing, from two different dates (by Invitae:)


So, particularly in the context of my most recent spinal imaging, (spoiler alert – it’s a mess) there’s especially concern with my deleted SMN1 gene, which is associated with SMA, a.k.a. Spinal Muscle Atrophy (not at allllll confusing when there’s SMAS, a.k.a. Superior Mesenteric Artery Syndrome, which I also have…) Apparently about 1 in 30 adults is a carrier, so it’s actually not all that rare. If two carriers mate, there’s a 25% likelihood SMA will manifest in their offspring.
The LPIN2 (associated with Majeed Syndrome) may also be of some concern, as it’s associated with bone inflammation, and carriers can exhibit things like psoriasis. The chronic skin irritation on my scalp may or may not be psoriasis. (There’s actually some good news on the top of the head front – I switched to a really pricey Aveda shampoo and changed the ingredients in my DIY “scalp rescue” remedy, and haven’t used the prescribed topical steroid for months!) The gene may also be associated (via something to do with anemia?) to multiple myloma, which my blood-related uncle had.
If you want any more information on these things, I’m happy to forward what I have. (I will also get more advice, and can keep you up to date.) There are notes on the Invitae testing and notes from a genetic advisor so far. The wait to see a geneticist at UC is years long – I think I’m on a “wait list to make an appointment” – and I hear they’re horrible with EDS, so I’m finding other ways to get genetic advice. For instance, Invitae offers a free counselling session with each test.
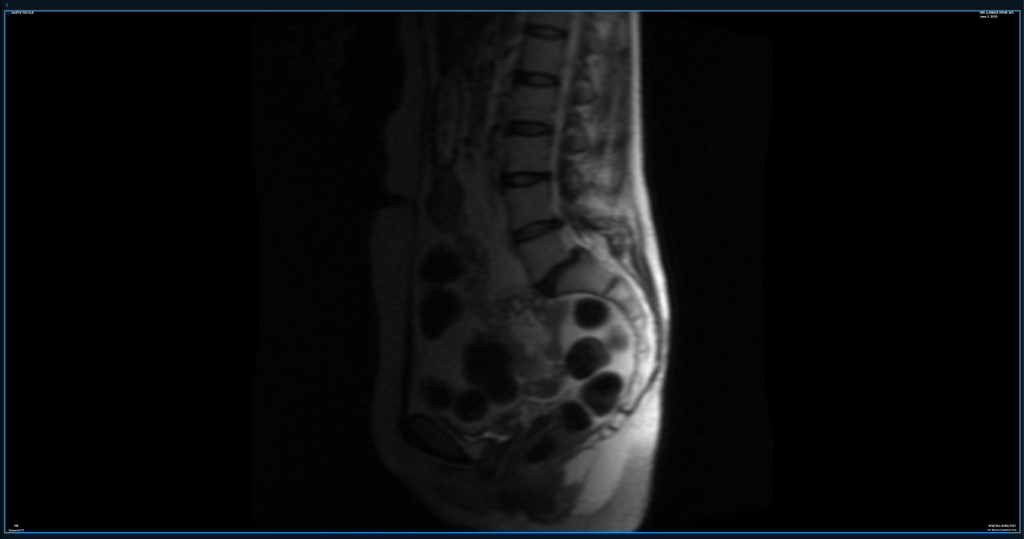
The Spine
I spent many hours in an MRI machine these past few months, for the fresh information and to get in the door with various specialists. I’ve had imaging of my pelvis and entire spine, and a brain MRI is upcoming. Pro tip: I upload all my imaging (when it works) to an online service, where it’s accessible and I can loop in docs with a simple email address (when they’re willing, which is maybe 50% of the time.) In any case, it keeps it all organized. I currently use MyMedical Images.com.
To sum up, there’s basically something – um, nefarious? – going on at about every level of my spine. The radiologist’s report is a thick jabberwocky of terms I stopped hi-lighting because the whole page was bleeding yellow. Things like “severe bilateral stenosis” stand out among several mentions of “bulging,” “thickening,” “pars defects,” “anterolisthesis” and my favorite word to say, “spodylolisthesis.” (“LOL” is right there in the word!) There’s also “kyphosis,” and many, many mentions of “protrusions” and “osteophytes” and “narrowing.” A scoliotic curve rounds it all out nicely.
The one bit of good news I thought I had to share was the radiologist did not see evidence of CSF leak, chiari malformation or tethered cord (kinda big deal spinal anomalies more common in EDSers than others.) One of my docs has strongly suspected 2-3 of these in recent months, which was one reason for multiple stints inside the MRI machine.
Niki, after twelve years in the vascular compression world, you’ve learned by now that radiologists look for certain things, and specialists see other things, right?
Well…I sat down with the new images with a new-ish doc. She’s an EDS specialist and very familiar with all the fun things hEDS has to offer, especially the spinal ones. We sighed, and I said, “Well, at least there’s no sign of CSF leak, chiari or tethered cord, right?” And she looked at me like, “Oh, sweetie…”
She then pointed out where my brain may be hanging low in the skull (“chiari malformation,”) where my spinal cord is falling lower than it should be within the spinal canal (“tethered cord”) and reminded me I have all the symptoms of a CSF leak, and it rarely shows up on imaging. She also had to explain – again – how in normal people the dura is a little like treated leather, which holds all that juicy spinal fluid inside, but in EDSers it can be more like cheesecloth, making the multiple leaks too miniscule to see on imaging – but present, nonetheless.
This could change my predicted surgery trajectory 180 degrees – in order to prevent more damage to my spine, we may need to surgically “untether” the spinal cord, inject some blood patches to seal the leak(s,) and who knows what else to fix this. Vascular compression surgeries may have to wait (which is kind of what I was doing, anyway? That or being a chicken.)
“And I’ve never been wrong,” she added, looking somehow simultaneously sympathetic and stern. OK. Deep breath. At least there’s a neurosurgeon she trusts not too far away in Bend, Oregon, where I’ve been wanting to explore for ages, anyway, right? It’s supposedly a paradise of fluffy, hippie, mountainous beauty. Bonus: Colin wants to go out there and explore for a future photo workshop. Road trip!!! I’d already called the office a couple months back (because we’d expected this result) and they’re booking only a few months out.
Alas, by the time the referral was sent to the wrong number several times, and I had the necessary imaging complete, that doc was no longer taking new patients.
So now I’m starting over. With a doc in Rhode Island.
“Oh, and see this part here, where your disks bulge posteriorly? That’s concerning to me, for, um, safety,” says the new-wish doctor. “Like if you were in a minor fender-bender, you could…” She makes a slashing motion across her neck with her hand. “You really have never seen an orthopedic spine specialist, in all these years?” Um, let me think about that. The file drawers in my head open. Colorado Springs? Flip-flip-flip…Maybe. Chicago? Flip-flip…Nope, I was still insured in Colorado when I lived there. New York? Flip… I don’t think so. It just was not a high priority, with everything else going on. For decades, I was sure there was something immunological going on. A parasite, an autoimmune disease…(I wasn’t wrong, but I wasn’t completely right, either.) Mental note to add an orthopedic spine specialist to the list. And not go bungie jumping any time soon.
So, several things could be going on with my spine. Some of these issues have been there for decades and I’m still standing, (literally,) so, like, no biggie. It was considered due to “hard living” before we knew I had hEDS. We could chalk some of it up to my 50+ years, but that’s really stretching it. More likely, my spine is very angry due to some combination of the loose ligaments associated with hEDS, being jerked around by the tethered cord, and possibly one of the genetic anomalies mentioned above.
To boot, this doc has noted my sacrum is “one for a case study,” in the abnormal way it curves, which naturally leaves my intestines in a bind (get it?) and isn’t playing nicely with the L-5 junction, not to mention my rectocele (prolapse at the perineum), at all. (Actually she thinks it may be L-6, as she suspects I have an extra vertebra, but now I’m boring you.)
I’d be remiss to not also mention a recent diagnosis of radial tunnel syndrome (like carpal tunnel, but at the elbow) in my right arm. I can feel it creeping into the left, as well. There is also a narrowing of the space where the nerves which work my arms come out of my neck.
This is why, if you’ve seen me play at a kirtan, you may have noticed I switch the harmonium from left-handed to right-handed every so often. My hands and arms are kinda weak, and whichever one is pumping the bellows gets especially tired. It helps to switch their duties up, but it does become a bit of a mess when we’re working in a tight space with delicately balanced octopuparian (is that a word? It is now…) system of cables, wires, music stands and microphones. My favorite is the creaking sound of re-hinging one side of the bellows when the microphone is turned way up. Reallllly subtle!
Surgeries / Procedures
Eagle Syndrome/sinus– Check. Though it ostensibly went well, there’s still a 20% chance we’ll need to decompress the left jugular vein in the future, as well. Most importantly, I’ve regained my ability to swallow and (perhaps more importantly for my ego) sing.
To answer the big question everybody asks, I’m not sure if the surgery benefitted me, overall, or not. Between the inability to swallow and stomach bug caught a month after surgery, I lost 20+ lbs. The weight loss may have exacerbated my NCS (renal nutcracker syndrome,) which makes eating hurt and, in turn, may have exacerbated my PCS (pelvic congestion syndrome) which creates pain in my lower abdomen and pelvis. Fluid dynamics in the body are complicated. It’s also possible I had increased pain because the impacted jugular had been acting as a gate, keeping blood from pooling in my lower body, and now that it’s open, blood may be getting congested, lower down.
I’ve since regained about half the weight, and much of these original issues have calmed down. This may be because my body is apparently pretty good at creating “collateral veins,” which are like smaller, alternate routes to a highway. These pathways are effective, but smaller and far less efficient – it takes more energy to pump blood through them than the main routes. It may also be because I may be one of those lucky people who gain weight just in the right spot – at the fat pad under the SMA angle – which helps support that renal vein and keep as much flow as possible going there (it’s mostly closed, but less closed is better than more).
My headaches have shifted, but not gone away altogether. Breathing through my nose feels like an ocean breeze – free and clear. Until I get a cold or allergies. And on the cold “front,” I got a cold a few weeks back and I believe it was the shortest, most mild cold I’ve had, maybe since childhood! I swear it was over in a week! I’m 50% convinced this has something to do with clearing decades of infection out of my face.
But we’d really hoped clearing that decades-old sinus infection would also calm down my inflamed tonsils. They have improved, but still look angry, and the right one has created a little extra lobe, reaching out to catch whatever I may throw at it. So one of the surgeries I’m currently also considering is tonsillectomy.
MALS (Median Arcuate Ligament) – I’ve chosen a surgeon in Salt Lake City, but am taking a pause. This surgery involves re-secting part of the diaphragm and stripping the celiac plexus back so pain doesn’t return. MALS is probably one of the main drivers of my pain, overall – since 1995 it’s felt like I have a broomstick piercing my torso, front to back, on the right side near the gallbladder. (And while my gallbladder isn’t working, we think at this point it is not creating this pain.)
The surgeon warns that 3-6 months of post-surgical nausea isn’t unusual, and I’m not sure I can stomach that – literally. I dread that spiral of weight loss, which exacerbates everything else. And perhaps more importantly, MALS surgery can exacerbate NCS (the organs invovled are very near to each other) and I don’t yet have a good surgical option for that.
Cholecystectomy (gallbladder removal) – Could be done along with MALS surgery, or separately. (My chosen MALS surgeon, Dr. Richards, prefers to do them separately, but others prefer to do them together.) My ejection fraction is like 17% so it’s not working, but may not be causing any issues, either. And I hold hope it could “rebound” with correction of other issues.
NCS (Renal Nutcracker Syndrome) – I’ve been rejected for my top option, AT (auto-transplant of the kidney, where they put your kidney lower down in your abdomen) or nephrectomy, at least by the local option at CU Denver. I was actually getting kind of excited about donating my left kidney….thinking about how much good I could do gave me a certain degree of warm fuzzies. But the transplant team here at UC Health, one of the most experienced in the world for this process for NCSers, felt that because my bladder pain spiked after their diagnostic Marcaine Cystoscopy, I may be one of those people who experiences long-term pain and UTIs from either procedure. Because the ureter gets cut…well, I’m a little unclear but apparently things can happen. And I already have a lot of bladder pain and dysfunction – I don’t want to make it worse.
The Colorado office is currently in collaboration with a team doing similar procedures in Madison, Wisconsin, and data may come out in the future which refutes this string of assumptions. But for now, the “committee” won’t approve me as a living donor because a) I have autoimmune disease, so my kidney is less desirable than most and b) we can’t prove the procedure would benefit me.
Are there other options? Yes, yes there are. LRVT (Left Renal Vein Transposition) has a high failure rate, and many go on to need AT. Internal stents tend to migrate, sometimes puncturing the aorta (not to mention the stents are dicey for those with metal allergies). Two docs in the US use an external stent made of PTFE, which is like Teflon, but one has a terrible habit of ignoring his patients after they present with complications, and the other is accessible but inconvenient – he doesn’t do telehealth outside of Texas. Many patients report nagging back pain after placement of these devices, and there’s no long-term data available on their effectiveness. A hybrid AT, where the kidney is dropped and the ureter not cut, may also be an option. I think there may be 2-3 surgeons in the world who offer this.
Dr. Kurtis Kim, vascular compression expert and advocate extraordinaire, currently has a thing coming out of his brain which may prove another good option – an internal PTFE stent which is stitched in place to prevent migration. Alas, he has been without a medical home for a couple years due to his (as best I understand it,) “spending too much time with his compression patients” and being asked to leave his practice. Litigation is involved, which I’m sure is just so great for his overall mental health and focus. I’ve consulted with him and he’s 100% THE guy, he just needs a few million bucks to get his vascular compressions one-stop shop/practice underway. If you happen to have that sitting around, give me a call – I have his number!
MTS (May-Thurner Syndrome) – Hopefully if I do the previous two surgeries, I won’t need this. It will self-correct. But it still may be a thing. Blood flow in the body is …unpredictable.
Celiac Plexus Block – the Diagnostic one felt SO good, but was only diagnostic and thus only lasted 24 hours. Since I’m putting off MALS surgery for now and I think the celiac plexus is a main generator of pain, I’m lobbying for one with steroids, which may last longer. Alas, EDSers tend to process steroid quickly, so it’s a TBD kind of potential pain therapy. Fingers crossed it could help.
Tonsillectomy – On the table, as my thorat is almost always sore and the tonsils look a chronically a little anrgy and gloopy, and the right one has made a little “annex” tonsil in front of itself.
Left Hip Labral Tear – I’ve been ignoring this for at least a decade, but at some point I’ll probably have to deal.
Tethered cord, chiari – TBD. Working on getting to the super-neurosurgeon in Rhode Island and I’ll see what she says.
CSF (Cerebrospinal Fluid) Leak – I’ll probably get a blood patch at some point, but the idea of needles in my spine isn’t exactly inviting. Before any intervention, I may try a 48 hour horizontal trial to see what happens. Apparently, occasionally that can seal a leak. There’s some inconvenient friction between my ENT (who can order a blood patch pretty quickly, but I hear isn’t completely trusted by the local neurosurgeons) and the UC neurologists, (who have a complex system of tiered docs and there’s a months long waiting list, but I may be able to skip over one tier by getting the correct imaging in front of the next tier, but they may be irritated with me if I work with the ENT at all…it’s, um, complicated.)
Overall, I’m in a gray area for most of these surgeries & procedures. I’m still capable of walking and eating, so I don’t crucially need any of them to survive. However, I do understand it also behooves one to behave as though one is going to survive long enough to suffer the repercussions of not correcting certain things earlier in life. And the optimal time for surgeries is, well, as long as you’re not a babe in arms…the younger, the better.
Meanwhile part of me feels I may, just may have this secret, backup plan…if I delay long enough, there’s….CRISPR! Gene editing tech is coming, people! If I understand correctly, there are children with muscular dystrophy getting some of their genes rearranged, as we speak. I’m also hearing about a human study for people with rheumatoid arthritis. If I had all this genetic tomfoolery eliminated, could some of the collateral damaged be halted, even reversed?
No one knows. That’s where we are.
Of course the sideshow for any woman, especially at this “special time of life,” is hormones. A DUTCH test showed my cortisol, which should spike in the morning, is flat-lined until about 5pm, explaining why I make no appointments before 2pm unless it’s an airplane which will leave without me. I’m exhausted, have difficulty sleeping, am hot, cold, irritable, hungry and cranky. My tank is almost completely empty of all the good stuff, like estrogen, progesterone and testosterone (yes, women need that, too) so now I’m “juicing” with all these things, thanks (I think) to yams, soybeans and pregnant mares?
(Side note: I have been hearing sporadic tales of people’s adrenal insufficiency clearing up completely, months after surgery for Renal Nutcracker Syndrome. I’m sure it’s a completely un-studied phenomenon, but a ray of hope, perhaps!)
And I must say, the Hashimoto’s (autoimmune hypothyroidism) journey is quite daunting, by itself. My last endocrinologist at least tried. This one is like, “If your blood levels aren’t off, don’t bother me.” She has zero curiosity about why an immune system would attack a perfectly good thyroid, creating a whole cascade of related events. (Yes, I voted this doc off the island yesterday. As Colin succinctly said, “She IS the weakest link!)
This is where functional medicine people show up to do the heavy lifting. I’m trying my darndest to stick to an autoimmune paleo diet, marrying it to a low histamine diet. (Plus my immunologist wants me off citrus for some damned reason.) The advice I’m now attempting to follow (and it is backed up by studies, I hear) is to eliminate all possible stress and toxins from my internal and external environments, including the teeniest chemicals in water (for drinking and bathing – looking into a reverse osmosis machine and a chlorine filter for the shower) pollutants in our air and chemicals in our food. Ack!
The alternative, I suppose, would be to move those of us who are “canaries in a coalmine” back a few centuries to before we had antibiotics, the internet, washing machines and “Wheel of Time” episodes on demand. I’m not sure I’d exactly be comfortable way back then. I’ve lived in developing places and I really do like those washing machines.
Want an interesting tidbit? One trending theory behind why autoimmune disease exists (and has been increasing in modern times) is because our ancestors survived things like the plague and the potato famine. People with immune systems on hyperdrive managed to survive the black death, and pass on their genes. People who were able to re-direct energy and slow metabolism in order to survive famine, now tend to manifest thyroid “issues,” such as weight gain, when under stress in modern times. And of course stress is so uncommon in modern times. 😉
It’s a lot to share, I know. From my perspective, these are a lot of big thoughts for someone with daily brain fog and only a few hours of energy every day. Each situation requires a deep dive into turbid waters, as this is just where we are in medical science right now. Each medication and supplement (there are about 30?) requires tracking for necessity, supply and price. (I’d thought maybe none of these meds were helping until I couldn’t swallow them for a couple months.) Some are compounded and have to be procured at a special pharmacy. Some are prescription but aren’t covered by insurance, so the web and the phones must be consulted for the best deals. Some are injected. (Learning to give myself shots with zero direction from the prescribing doc was quite the adventure, but now I like to think I’m quite good at it!) Some come by mail. Some are controlled, so can’t be automatically refilled and require several phone calls to manifest. (Especially tricksy when your PCP is on maternity leave.) For some, insurance will only pay for a 45 day supply, so they can’t all possibly be coordinated in any way with the ones which are doled out in a 90 day supply, resembling nothing like a streamlined solution.
And, of course, all my docs disagree about which meds I should take, which diet I should be on, which surgeries I should do and in which order. So, into the deep of the web I go, reading studies, (to the extent I can pay attention, and my neck and eyes will allow) reading conflicting studies, (I’m a glutton for punishment and a general gnashing of teeth) talking with other patients, delving equally into scientific skepticism and intuition, using meditation and chant practices for patience, clarity and balance.
I celebrate the small victories, like getting the right prescription to the right pharmacy after weeks of phone calls. Peaches growing on our new tree. A good hair day. The hours after a massage where I remember what a body feels like when it’s untethered. Singing like no one’s listening with my kirtan group. Pushing a produced song out, like a crying babe into the world, whether the world cares about it or not.
You know how you read your resume and suddenly think, “Oh, I’ve done a bunch of really cool stuff! I must be so smart and capable!” I recently participated a study on the economic impact of EDS. As I tallied it up, looking at the sheer number of hours and dollars I put into medical care on a weekly and annual basis was…eye-opening.
Here’s another related, succinct Colin-ism: “So, you spend about fifty percent of your energy trying to get more energy.”
That’s about right.








Leave a comment